The nasal valve is a term used to describe the narrowest part of the nose internally. This is the area that determines if someone feels normal or obstructed breathing through the nose. When this area is overly narrowed and blocked, we call it nasal valve collapse.
There really are two types of nasal valve collapse. The collapse of the tip cartilages described above can cause external valve collapse where the blockage is just past the nostril. When most surgeons discuss valve collapse, though, they are talking about internal valve collapse. This occurs when the upper lateral cartilages in the middle of the nose have been too narrowed. This problem happens when a nasal bump is taken down too much and when the cartilages themselves are shortened or not reattached during a Rhinoplasty. The problem seems to occur more often after a closed Rhinoplasty because most surgeons detach these cartilages without repairing and reattaching them at the end of the procedure. When the natural cartilage supports have been lost, they simply fall inwards and collapse. The result is poor breathing and two visible cosmetic deformities. One is called an ‘inverted V deformity’. That’s because the collapsed area where these cartilages attach to the nasal bones looks like an upside-down letter V. The second problem is that the middle part of the bridge can start to look very pinched.
http://www.rhinoplastyinbeverlyhills.com/rhinoplasty-mistake-8-nasal-valve-collapse
Dr. Craig Murakami explains that an internal nasal valve is considered to have collapsed when the angle of the valve is less than 10[degrees] to 15[degrees]. Its etiology can be congenital, traumatic, or iatrogenic. (1) In the latter case, collapse is often caused by over-resection of the nasal dorsum and upper lateral cartilages during septorhinoplasty. Such an overly aggressive operation can result in concurrent dorsal concavity (saddle-nose deformity) or a narrowing of the middle third of the nose (hourglass deformity).
http://findarticles.com/p/articles/mi_m0BUM/is_3_83/ai_n6077596/
Important nose anatomy illustration diagrams from Dr. Beckers website.
Rhinoplasty, Postrhinoplasty Nasal Obstruction
Author:Thomas Romo III, MD, FACS
Coauthor(s): James M Pearson, Haresh Yalamanchili, MD, Paul Presti M.D.
Grymer used acoustic rhinometry to evaluate the internal dimensions of the nasal cavity in 37 patients before reduction rhinoplasty and again 6 months after surgery.3 He demonstrated that rhinoplasty decreases the cross-sectional area of the nasal valve by 25% and the piriform aperture by 13%. Cole et al also used rhinomanometry to reveal that changes of as small as 1 mm to the nasal valve size can dramatically increase nasal resistanceTherefore, the nasal valve, as a regulator of nasal airflow and resistance, has been demonstrated to play a critical role in the function of the nose. Disturbance of the nasal valve area can produce limitations to normal nasal breathing. Multiple schemes can be used to classify the types of nasal valvular dysfunction. One convenient method is to group them according to either internal or external nasal obstruction (see Classification of nasal valve dysfunction). Kern and Wang divide the etiologies of nasal valve dysfunction into mucocutaneous and skeletal/structural disorders. The mucocutaneous component refers to the mucosal swelling (secondary to allergic, vasomotor, or infectious rhinitis) that can significantly decrease the cross-sectional area of the nasal valve and thus reduce nasal airway patency. The skeletal component can be further divided into static and dynamic nasal dysfunction.
In summary, nasal valve dysfunction can be secondary to either mucocutaneous problems or skeletal deformities (affecting either the internal or the external nasal valve), which can be dynamic or static. However, the cause is rarely so straightforward. In most instances, the mucocutaneous and skeletal components and the static and dynamic components contribute in varying degrees to the overall nasal valvular dysfunction.
Skeletal deformity:
Deformities that affect the internal nasal valve area
- Static deformity
- Inferomedially displaced upper lateral cartilage
- Narrowing of pyriform aperture
- Scarring at intercartilaginous junction
- Turbinate hypertrophy
- Deviated nasal septum
- Dynamic deformity - Collapsed upper lateral cartilage secondary to disruption of support from the nasal bone, septum, and lower lateral cartilage
The internal nasal valve area is the narrowest portion of the nasal passage and thus functions as the primary regulator of airflow and resistance. The cross-sectional area of the nasal valve area is 55-83 mm2. As described by the Poiseuille law, airflow through the nose is proportional to the radius of the narrowest portion of the nasal passageway, raised to the fourth power. Thus, changes as small as 1 mm in the size of the nasal valve exponentially affect airflow and resistance through the nasal cavity.
http://emedicine.medscape.com/article/841574-overview#Classificationofnasalvalvedysfunction
Rhinoplasty, Internal Valve Stenosis
Author: David Núñez-Fernández, MD, PhD Co-Authors: Jan Vokurka, MD, PhD, Gloria Fernández-Muñoz, MDThe airflow resistance provided by the airways during breathing is essential for good pulmonary function. The nose is responsible for almost two thirds of this resistance. Most of this resistance occurs in the anterior part of the nose. This region is called the nasal valve, and it acts as a flow-limiter.
External nasal valve collapse can be found in patients without a history of trauma or surgery. These patients commonly have an overprojecting nose with extremely narrow nostrils. Another cause can be an extremely wide columella,
Internal nasal valve collapse can be divided depending on the structure that caused the collapse. In many cases, more than one structure is affected. The most common cause is probably septal deviation. The second cause is collapse secondary to rhinologic surgery, especially after removal of the nasal roof. Khosh found, in 53 patients, the following causes of nasal valve collapse: previous rhinoplasty (79%), nasal trauma (15%), and congenital anomaly (6%).4
Upper lateral cartilage (ULC)
Thickened cartilage can compromise an adequate aperture. The cartilage can also be twisted, deflected, or associated with excessive return of the caudal border. An absence of cartilage, either congenital or iatrogenic, can produce a flaccid valve that collapses during inspiration.
Lower lateral cartilage (LLC)
Overresection during rhinoplasty can weaken the cartilage and cause inspiratory collapse. Deformation of the cartilage can be a result of trauma or congenital malformations of the cartilage.
Although uncommon, some patients may have deformities of the pyriform aperture that reduce the space of the nasal valve.
Rhinoplastic procedures are particularly prone to disturbing the nasal valve area. Hump removal affects the nasal valve in several ways. If the hump is particularly large, separation of the ULC can be necessary. Resection of the T-shaped area of the dorsal border of the septum produces a narrower area in the roof. If the mucosa in the valve is not protected during the surgery, which occurred with the use of many older techniques, scarring of the valve can lead to structure formation or stenosis of the valve.
In reduction rhinoplasties, the cross-sectional area of the overall nose is reduced. This increases the resistance to airflow. If the nasal valve is not properly repaired during the surgery, patients may report nasal obstruction after the surgery, even if this was not reported preoperatively. Overresection of the lower lateral cartilage can lead to pinching and inspiratory collapse.
Because it is the narrowest part of the nose, the nasal valve can be affected by minute alterations of the nasal anatomy that would not be important in other areas.
The angle between the ULC and the nasal septum is 10-15° (normally in Caucasians). Internal nasal valve collapse occurs when, for some reason, this angle is diminished. The result is an increase in nasal resistance to airflow; consequently, the patient reports nasal obstruction. The opposite is known as ballooning. In this case, the nasal valve is excessively open.
The pyriform aperture continues the limit of the valve from the ULC to the floor. The head of the inferior turbinate is immediately posterior to the pyriform aperture and plays an important role in the function of the valve, which is the reason it is also considered part of the internal nasal valvehttp://emedicine.medscape.com/article/877468-overview
Identifying nasal valve dysfunction:
Diagnosis can be difficult if the physician does not visualize the valvular area. Examining the valve without disturbing it with a nasal speculum is important because the speculum usually opens the valve. Sometimes, trimming the vibrissae is necessary to obtain a clearer view of the valve. Another method is to use a 0° endoscope
The Cottle test is useful to evaluate nasal valve stenosis. The cheek of the evaluated side is gently pulled laterally with 1 or 2 fingers, which opens the valve.
NOTE: Cottle test can be nonspecific
The problem with the standard Cottle maneuver is the results can be nonspecific. Dr. Jack D.Sedwick mentions on his website that a straightforward narrowing of the nasal airway produced by septal deviation or turbinate hypertrophy is improved by the Cottle maneuver. Anterior rhinoscopy is also a poor means of accurately evaluating subtle changes in nasal valve anatomy; the dysfunctional nasal valve can be missed due to distortion from the nasal speculum.
A more precise diagnosis can be made based on direct inspection of valvular support during quiet and forced inspiration. Collapse at the internal nasal valve is usually diagnosed based on the identification of medialization of the caudal margin of the upper lateral cartilages due to negative pressure created upon inspiration through the nose. A fine swab or cerumen curette may be used to lateralize the upper lateral cartilage to confirm the presence of internal valvular collapse.
More recently, Hilberg et al introduced acoustic rhinometry as a noninvasive and reliable objective method for determining the cross-sectional area of the nasal cavity.7 Acoustic rhinomanometry is based on the analysis of sound waves reflected from the nasal cavities.
Also, analysis can be done before and after topical decongestants are applied, allowing discrimination of mucocutaneous versus structural blockage. Standards for age, race, ethnicity and sex have been recently published.
http://www.providence.org/alaska/medstaff/nasalvalve.htm
http://emedicine.medscape.com/article/841574-overview#Classificationofnasalvalvedysfunction
http://simple-med.blogspot.com/2009_02_01_archive.html
Click on diagrams below for larger view
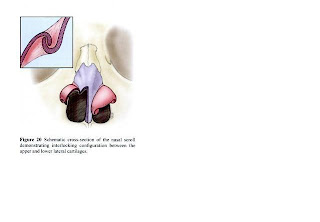 |
| Note: Insert Picture, Upper and Lower Lateral Cartilage scrolls interlocking |




No comments:
Post a Comment